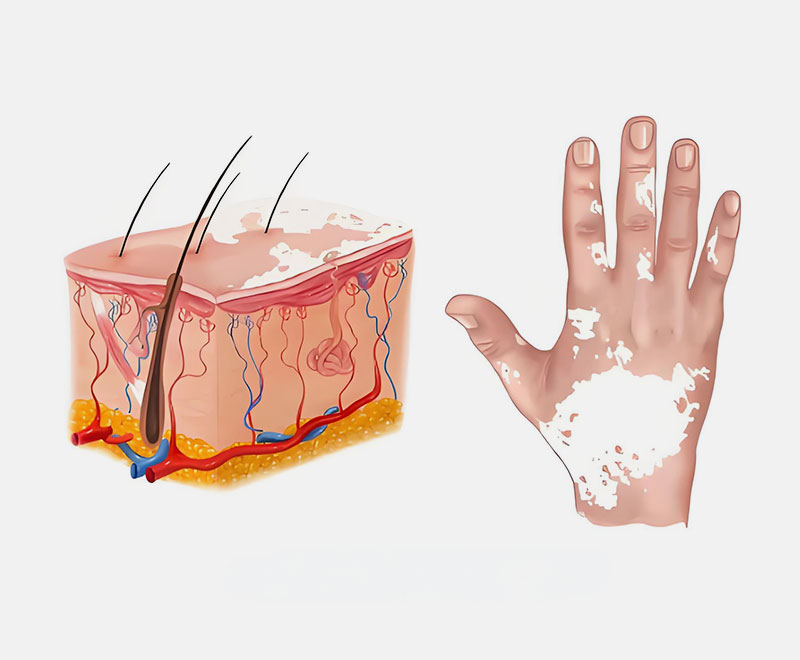
Vitiligo is a pigmentary disorder of the skin caused by the destruction of melanocytes. It is currently believed to be an autoimmune disease, commonly affecting areas such as the face, hands, and joints—especially regions exposed to friction. The hallmark of vitiligo is well-defined white patches of varying sizes, with a smooth surface free of scales and usually without itching, pain, or other discomfort.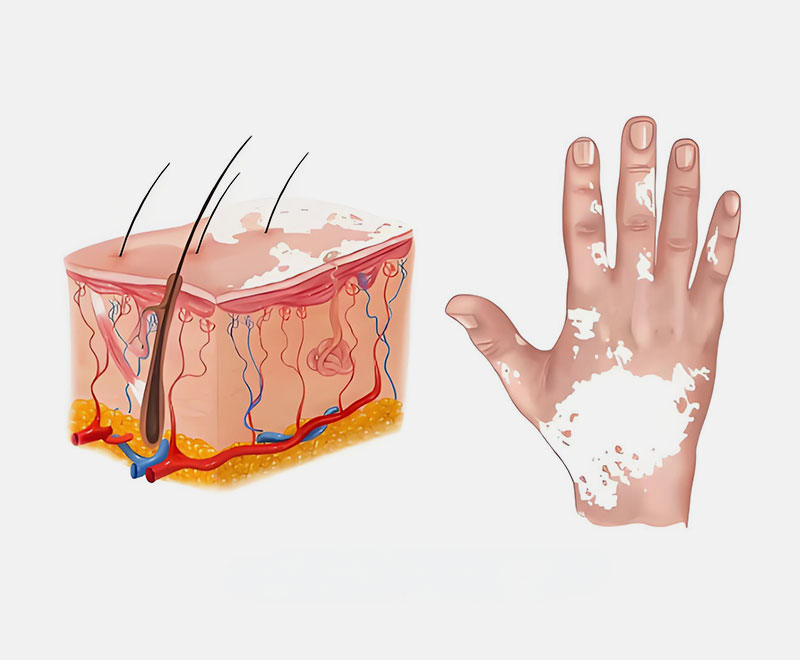
Disruption in Melanin Production Due to Melanocyte Destruction
Treatment of vitiligo mainly depends on the classification and staging of the condition, employing various therapeutic approaches. These include systemic or topical corticosteroids, calcineurin inhibitors, vitamin D3 derivatives, traditional Chinese medicine, phototherapy, transplantation therapy, depigmentation therapy, and camouflage therapy.
Photochemotherapy (PUVA)
Photochemotherapy, or PUVA, is a traditional phototherapy method that uses photosensitizers to enhance the effectiveness of UV treatment in skin diseases. It increases the activity and number of melanocytes in vitiligo patients. For widespread lesions, patients take 8-MOP orally and then undergo long-wave UV exposure until erythema develops. For localized lesions, topical psoralen is applied before UV exposure or sunlight. Treatment is typically administered 2-3 times a week.
Potential side effects of PUVA include burns, nausea, erythema, itching, xerosis, fatigue, carcinogenicity (including melanoma), pigmentation damage, cataracts, and aging. PUVA is contraindicated in pregnant and breastfeeding women, those with a history of skin cancer, arsenic or radiation therapy, Roentgen-ray exposure, photosensitivity disorders, or cataracts.
PUVA, once the most common treatment, is increasingly being replaced by NB-UVB and 308nm excimer light/laser for vitiligo treatment.
Narrowband Ultraviolet B (NB-UVB)
NB-UVB therapy works by inducing the proliferation of inactive melanocytes in the hair follicle outer root sheath and stimulating melanin production and migration to depigmented areas, thus restoring pigmentation. Its immunosuppressive effect prevents the destruction of newly formed melanocytes.
Micro NB-UVB phototherapy is suitable for localized vitiligo, while whole-body NB-UVB therapy is used for disseminated or generalized vitiligo. Treatments are typically administered 2-3 times a week, with different initial dosages selected based on the treatment area or determined by minimal erythema dose (MED) testing. The starting dose is 70% of the MED. The dosage for the next session depends on the erythema response to the previous session. The efficacy of NB-UVB treatment does not necessarily increase with the number of treatments, frequency, erythema dose, or cumulative dose. Furthermore, higher cumulative doses increase the likelihood of side effects such as dry skin, itching, and photoaging.
308nm Excimer Light/Laser
The 308nm excimer light/laser emits a single wavelength of 308nm, generated using xenon chloride gas. This wavelength is close to that of NB-UVB but with 5-10 times the energy. It activates differentiation, maturation, and migration of melanocyte stem cells in the hair follicle and skin, as well as inducing T-cell apoptosis, promoting repigmentation of white patches. The 308nm excimer light/laser is currently the most advanced phototherapy technique for vitiligo and the only phototherapy device approved by the FDA for vitiligo treatment.
The 308nm excimer light/laser is suitable for patients of all ages, from infants to the elderly, as well as special populations such as pregnant women. It can be safely used to treat sensitive areas, including the eyelids, lips, external genitalia, and perianal region. However, patients with photosensitivity disorders should avoid this treatment. Treatments are typically administered 2-3 times a week, with potential erythema at the treated area that usually subsides within 24-48 hours.
Combination Therapy with Phototherapy
In clinical practice, phototherapy is often combined with other treatments to achieve better results. Common combinations include phototherapy with systemic or topical corticosteroids, topical calcineurin inhibitors, oral traditional Chinese medicine, topical vitamin D3 derivatives, topical photosensitizers, transplantation therapy, oral antioxidants, fractional laser therapy, and dermabrasion.
Home Phototherapy
Home phototherapy allows patients to use professional phototherapy devices at home under the guidance of a physician. Patients should receive professional instruction, understand the use of home phototherapy devices, and be familiar with their phototherapy regimen and dose adjustment principles, enabling safe and effective treatment outside the clinic.
Selection of Home Phototherapy Devices
- To reduce safety risks, patients should purchase phototherapy devices approved by the National Medical Products Administration (NMPA) with a valid medical device registration certificate explicitly indicating their suitability for home use.
- The selection of the device should be based on the size and location of the lesions. For large or generalized lesions, a half-body phototherapy device is recommended. Portable devices are suitable for smaller areas. Specific areas may require specially designed devices or accessories, such as a treatment comb for scalp lesions.
- Patients are advised to choose home phototherapy devices that can directly set the dose or have a built-in automatic timer to avoid overexposure.